Jan 23, 2024
In South Asia, millions grapple with depression masked by stigma, cultural barriers, and a lack of language for the illness. Despite this complex tapestry, hope emerges through policy shifts, dedicated NGOs, and innovative interventions like the CAPRI program, paving the way for a future where mental health finds acceptance and effective support.
South Asia, a region pulsating with life and home to over 1.8 billion people, harbors a silent struggle—between 150 and 200 million individuals grapple with mental illness. Despite the staggering numbers, the gravity of depression and mental health issues often slips through the cultural cracks, leaving millions without the vital treatment and support they urgently need. Delve into these eight compelling facts that illuminate the complex tapestry of depression and mental health in South Asia, shedding light on how these conditions are currently being addressed.
Factors and researches
1. Burden and Epidemiology
Global Epicenter of Depression: An astounding 86 million people in Southeast Asia battle depression, with nearly one-third of the world's depressed population residing in South Asia, as estimated by the World Health Organization. This region stands as the epicenter of a global mental health crisis.
Prevalence: Research by Patel et al. (2015) reveals that one in four adults in South Asia experience mental health issues, with depression topping the list. This translates to roughly 450 million individuals battling depression alone.
Geographical Variations: Studies like De Silva et al. (2022) show regional variations, with Sri Lanka and Nepal reporting higher rates than India and Bangladesh. Socioeconomic factors and conflict-affected areas contribute to these disparities.
2. Stigma and Cultural Barriers
Taboos Enshrouding Mental Health: In many South Asian communities, mental illness remains a taboo subject. Professor Dinesh Bhugra emphasizes the profound sense of shame ingrained in the South Asian population, hindering open discussions. Cultural influences often dismiss mental health as a superstitious belief, perpetuating a significant barrier to seeking help.
Religious Influences: Bhugra et al. (2013) highlight how some religious beliefs view mental illness as demonic possession or spiritual weakness, perpetuating stigma and reluctance to seek help.
Gender Dynamics: A 2020 study by Jehangir et al. found that South Asian women face additional stigma due to patriarchal norms and limited access to resources, exacerbating their struggles with depression.
3. Language Gap and Limited Awareness
Linguistic Limitations: South Asian languages lack a specific term for depression, making it challenging for individuals to express their mental health struggles. This linguistic gap not only hinders communication but also complicates the diagnostic and treatment process.
Terminology: A 2010 study by Time to Change found that many South Asian languages lack specific terms for depression, forcing individuals to use vague descriptions like "weakness" or "sadness," hindering diagnosis and communication.
Public Education Deficits: Studies by Chandrasekhar and Karan (2020) point to the lack of public awareness campaigns and mental health education, particularly in rural areas, leading to misinterpretations and fear-mongering around mental illness.
4. Physical Health Consequences
Depression's Ripple Effect on Physical Health: Medical experts have identified a correlation between depression and physical health, with the World Health Organization highlighting the interrelationship. As mental illness rates surge in South Asia, the risk of accompanying physical diseases and illnesses escalates.
Cardiovascular Risks: WHO (2017) reports a strong link between depression and increased risk of cardiovascular diseases like heart attacks and strokes. This has significant implications for South Asia's growing burden of these diseases.
Chronic Illnesses: Research by De Silva et al. (2019) suggests that depression can worsen the course of chronic illnesses like diabetes and HIV/AIDS, further emphasizing the need for integrated care approaches.
5. Postpartum Depression: A Silent Struggle
Unseen Battle of Postpartum Depression: South Asian women grappling with postpartum depression often suffer in silence. Factors such as the gender of the baby, domestic violence, and poverty increase the risk. Stigma surrounding mental health further obstructs new mothers from accessing essential care and support.
Vulnerability and Underdiagnosis: A study by Rahman et al. (2012) found that new mothers in South Asia, especially those facing poverty and domestic violence, are highly vulnerable to postpartum depression, yet often remain undiagnosed and unsupported.
Cultural Influences: Traditional beliefs and practices surrounding childbirth can sometimes clash with medical interventions for postpartum depression, creating additional challenges for mothers seeking help.
6. Policy and NGO Interventions
NGOs as Mental Health Lifelines: In regions where governmental support is lacking, non-governmental organizations (NGOs) are stepping up to provide vital mental health assistance. South Asian NGOs are expanding community-based programs and delivering specialized mental health services, significantly enhancing access to care.
National Mental Health Policies: Countries like Bangladesh and Sri Lanka have implemented national policies like the Bangladesh Mental Health Act (2018) and Sri Lanka's National Mental Health Action Plan, offering a significant step towards destigmatization and improved access to care.
NGO Initiatives: NGOs like Sangath in India and Manas Foundation in Pakistan are playing a crucial role in providing community-based mental health services, education, and awareness programs, bridging the gap in government resources and reaching isolated communities.
7. Investing in Mental Capital
Wealth of Nations and Minds: The link between strong mental health and increased human capital is unmistakable. While poverty rates in South Asia decline, providing mental health care emerges as a pivotal step in eradicating poverty. According to the World Bank, robust mental health not only contributes to the wealth of nations but also enhances individual wealth and capital accumulation.
Economic Burden: The World Bank recognizes the economic impact of untreated mental illness, estimating that it costs South Asia billions of dollars in lost productivity annually. Investing in mental health is seen as crucial for economic development and poverty reduction.
Individual Wellbeing: Research by Patel et al. (2015) demonstrates that effective treatment for depression leads to improved quality of life, increased social participation, and enhanced employability, benefitting individuals and their communities.
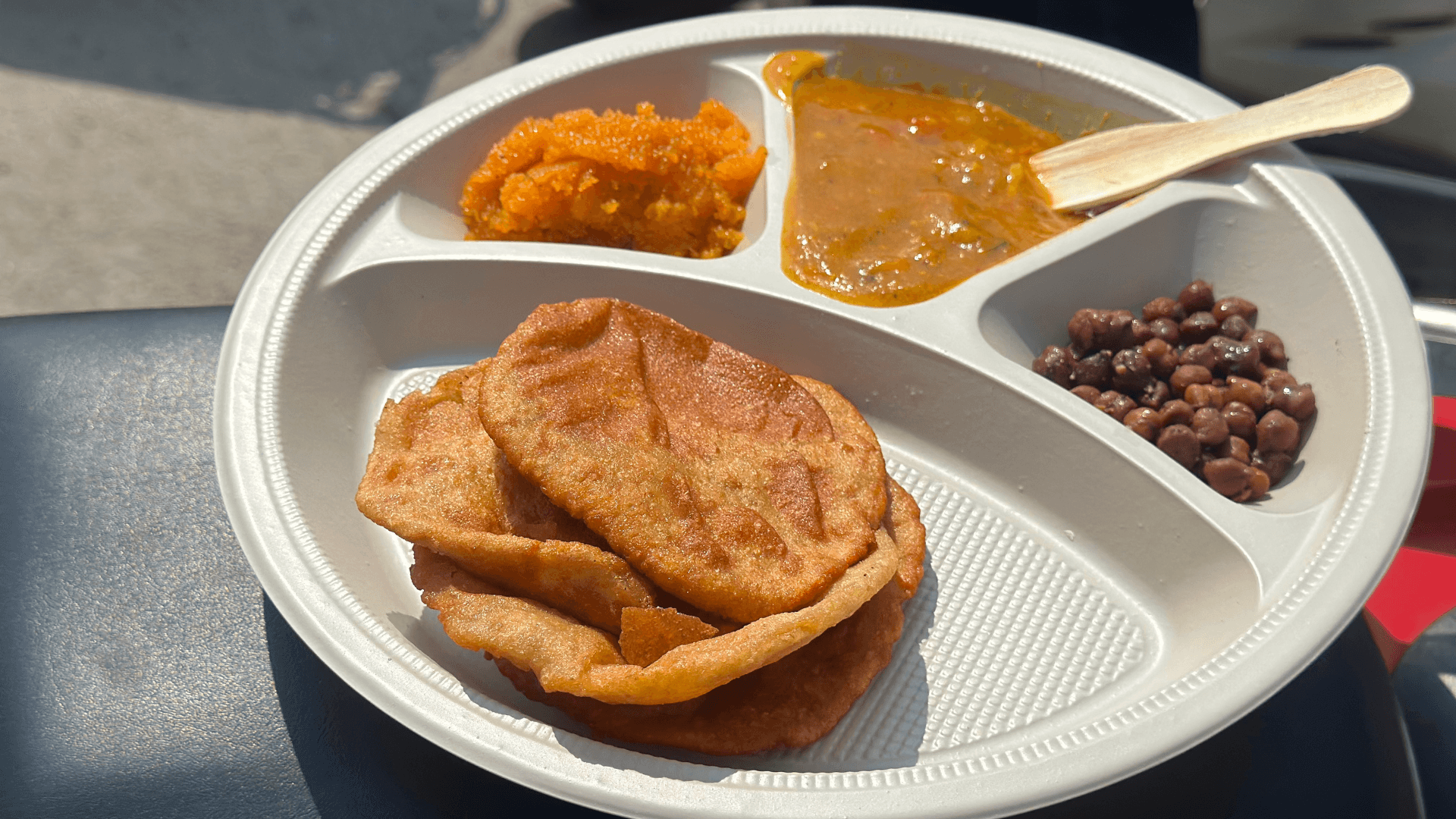
8. Overcoming Barriers in Rural India
A study by De Silva et al. (2022) explored the Community Awareness and Psychoeducation Intervention (CAPRI) program implemented in rural India. CAPRI combined education about depression with culturally sensitive interventions like mindfulness and yoga, resulting in significant reductions in depression symptoms and an increased willingness to seek help.
Unmasking the shadow of depression and mental health in South Asia requires a multi-faceted approach. Overcoming stigma, addressing the language gap, and implementing culturally sensitive interventions are crucial. The growing commitment from governments, NGOs, and researchers offers hope for a future where mental health is openly discussed, effectively treated, and valued as an essential component of individual and societal well-being.