Feb 19, 2024
The study published in BMC Family Practice (2023) conducted a systematic review to identify factors contributing to the inappropriate use of antibiotics in South Asia. Analyzing data from various levels (patient, provider, healthcare setting, community, and policy), the study highlights the complexity of the issue and emphasizes the need for multi-sectoral interventions to promote responsible antibiotic use.
Antimicrobial resistance (AMR) is a pressing global health concern, and South Asia is not immune to its effects. With a dense population, inadequate healthcare infrastructure, and widespread misuse of antibiotics, the region faces significant challenges in combating AMR.
The revolutionary discovery of antibiotics in the 19th century transformed medicine, offering a powerful weapon against bacterial infections. However, the overuse and misuse of these life-saving drugs have had unintended consequences. Bacteria have evolved resistance mechanisms, rendering once-effective antibiotics useless. This phenomenon, known as antibiotic resistance (AR), has emerged as a global public health threat, with South Asia facing a particularly high burden.This article explores the factors contributing to AMR in South Asia and discusses potential solutions to mitigate its impact.
The Rise of AMR in South Asia
South Asia, comprising countries such as India, Pakistan, Bangladesh, Sri Lanka, Nepal, and Bhutan, is home to over a quarter of the world's population. The region grapples with a high burden of infectious diseases, including tuberculosis, malaria, and diarrheal illnesses. Antibiotics are frequently prescribed to treat these infections, but inappropriate use, including over-prescription, incomplete treatment courses, and the availability of antibiotics without prescription, has fueled the emergence of AMR.
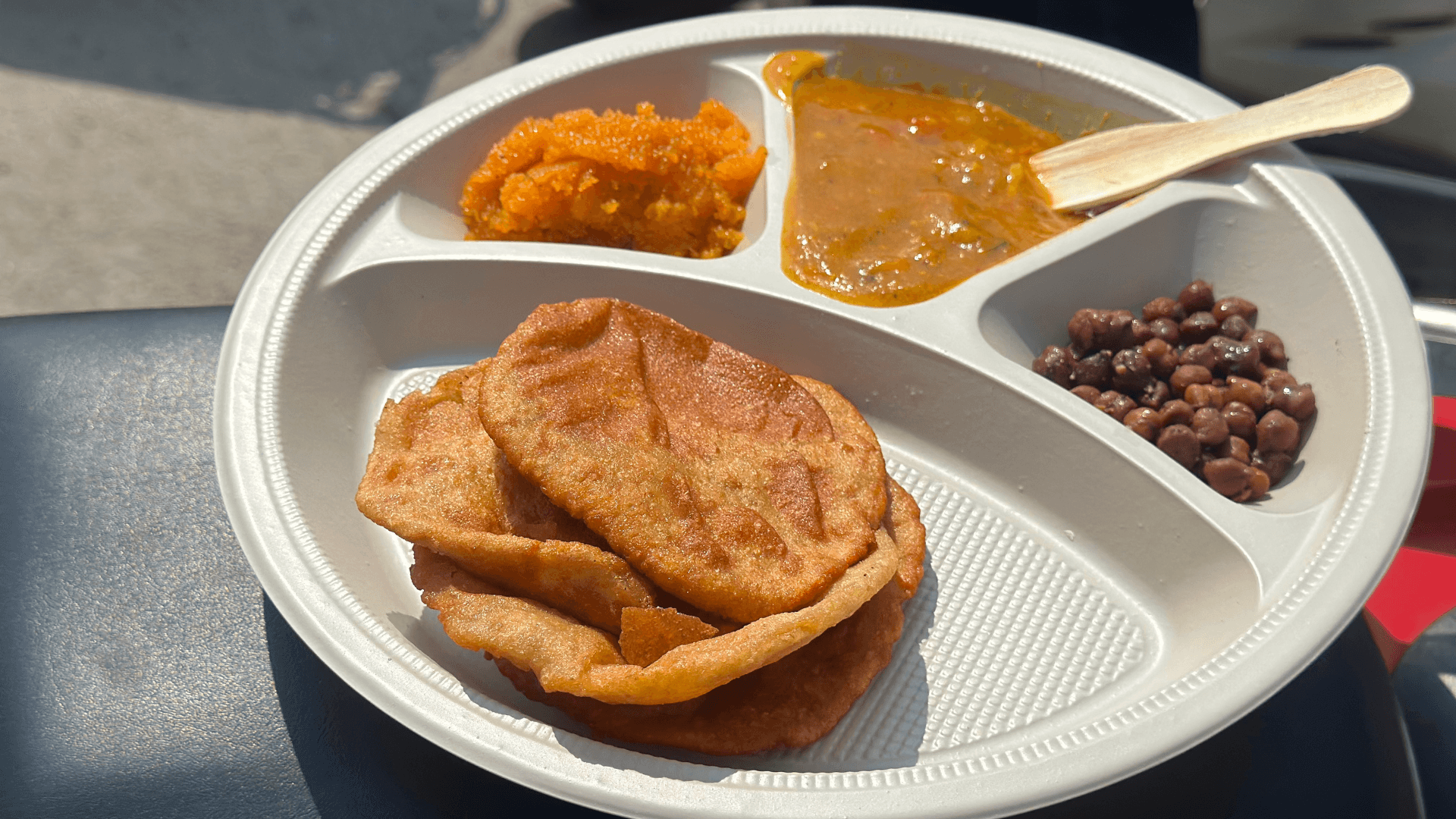
One of the primary drivers of AMR in South Asia is the widespread use of antibiotics in agriculture and animal husbandry. In countries like India, antibiotics are often used as growth promoters in livestock farming, contributing to the dissemination of resistant bacteria through the food chain. Additionally, inadequate sanitation and hygiene practices facilitate the transmission of resistant pathogens in communities, exacerbating the AMR problem.
Alarming Statistics:
High Prevalence: Studies indicate alarmingly high rates of resistance in South Asia. A review of data from 11 countries in the World Health Organization's (WHO) South-East Asia Region found resistance rates exceeding 33% for commonly used antibiotics against urinary tract infections.
Worrying Trends: Despite increased awareness and action, several countries, including Bangladesh, India, and Sri Lanka, report a worrying trend of increasing drug resistance. This indicates the urgent need for more effective interventions.
Economic Burden: AMR poses a significant economic burden on the region. It prolongs illnesses, necessitates expensive alternative treatments, and increases healthcare costs, impacting both individuals and healthcare systems.
76.8 deaths per 100,000 in South Asia are attributed to AR, highlighting its significant impact on mortality.
Studies reveal alarmingly high resistance rates exceeding 33% for commonly used antibiotics against urinary tract infections in several South Asian countries.
Uncontrolled antibiotic use in livestock production is a major contributing factor to the rise of AR in the region. The poultry industry has witnessed exponential growth, leading to intensive farming practices. To meet the increasing demand, farmers often resort to heavy antibiotic use in poultry for various reasons:
Treating existing illnesses
Preventing potential infections
Promoting faster growth (although the exact mechanism remains unclear)
This injudicious use has dire consequences:
Antibiotic-resistant bacteria :
Antibiotic-resistant bacteria develop and spread through various pathways:
Contaminated poultry products: Improperly handled or cooked poultry meat can harbor resistant bacteria, which can enter the human body through consumption.
Environmental dissemination: Antibiotics used in livestock farming can contaminate soil and water bodies, creating reservoirs for resistant bacteria.
Horizontal gene transfer: Resistant bacteria can share their resistance genes with other bacteria, further accelerating the spread of AR.
Unregulated Antibiotic Use: The widespread availability and over-the-counter sale of antibiotics in many South Asian countries contribute to their misuse and overuse. This fuels the development and spread of resistant bacteria.
Weak Antimicrobial Stewardship: Lack of proper prescription guidelines and adherence to antimicrobial stewardship programs in healthcare settings further exacerbate the problem.
Antibiotic Use in Livestock: The extensive use of antibiotics in animal husbandry as growth promoters or disease preventatives creates another major reservoir of resistant bacteria, contaminating the food chain and environment.
Example: The Case of Multidrug-Resistant Tuberculosis (MDR-TB):
MDR-TB is a form of tuberculosis resistant to several first-line antibiotics, making it significantly more difficult and expensive to treat. South Asia has emerged as a global hotspot for MDR-TB, with India alone accounting for nearly a quarter of the world's cases. This poses a serious threat to public health, as MDR-TB requires longer and more complex treatment regimens, increasing the risk of treatment failure and transmission.
Challenges in Addressing AMR
Several challenges impede efforts to address AMR effectively in South Asia. Weak regulatory frameworks contribute to the unrestricted sale of antibiotics without prescription, enabling self-medication and inappropriate use. Limited access to quality healthcare services and diagnostics further exacerbates the problem, as patients may resort to over-the-counter antibiotics without proper medical guidance. Moreover, the lack of awareness among healthcare providers and the general public about the implications of AMR hampers prevention and control efforts.
Inadequate surveillance systems also pose a significant challenge in monitoring the spread of resistant pathogens and guiding treatment strategies. Many countries in South Asia lack comprehensive data on antibiotic consumption patterns, resistance prevalence, and healthcare-associated infections, hindering evidence-based decision-making.
Mitigating AMR: A Multi-Faceted Approach
Addressing AMR in South Asia requires a multi-faceted approach involving collaboration between governments, healthcare professionals, the pharmaceutical industry, and civil society. Here are some key strategies:
Strengthening Regulatory Oversight: Governments should enforce regulations to restrict the over-the-counter sale of antibiotics and promote rational prescribing practices. Implementing and enforcing guidelines for antibiotic use in healthcare facilities and agriculture is essential to curb misuse.
Improving Access to Healthcare: Investing in healthcare infrastructure, particularly in rural areas, can improve access to quality healthcare services and reduce reliance on self-medication. This includes expanding the availability of diagnostic tests to ensure accurate diagnosis and appropriate treatment.
Enhancing Surveillance and Data Collection: Establishing robust surveillance systems to monitor antibiotic use, resistance patterns, and healthcare-associated infections is crucial for informed decision-making. This requires collaboration between health authorities, laboratories, and research institutions to collect and analyze comprehensive data.
Promoting Public Awareness: Raising awareness about the prudent use of antibiotics and the consequences of AMR is essential to change behavior among healthcare providers and the general public. Educational campaigns targeting both urban and rural populations can empower individuals to make informed choices about antibiotic use.
Encouraging Research and Innovation: Investing in research and development of new antibiotics and alternative treatment modalities is vital to combating AMR in the long term. Governments should incentivize pharmaceutical companies to invest in developing novel antimicrobial agents while promoting stewardship programs to optimize their use.
Conclusion
Antimicrobial resistance poses a significant threat to public health in South Asia, exacerbated by factors such as overuse of antibiotics, weak regulatory frameworks, and inadequate healthcare infrastructure. Addressing AMR requires a concerted effort from governments, healthcare providers, and society as a whole. By implementing comprehensive strategies to promote rational antibiotic use, strengthen surveillance systems, and raise awareness, South Asia can mitigate the impact of AMR and safeguard the effectiveness of antibiotics for future generations.