Feb 16, 2024
Fifteen studies conducted across diverse high-income countries were included in the analysis. The prevalence estimates of clinically significant symptoms of postpartum depression (CSS-PPD) exhibited considerable variation, ranging from 1.9% to 52%, with the most prevalent estimates falling within the 5% to 20% range. Among overseas-born women, particularly those from South Asian backgrounds, approximately five studies observed a doubling in the risk of CSS-PPD, with Odds Ratios ranging from 1.8 to 2.5.
The higher prevalence of postpartum depression (PPD) among South Asian women compared to the general population demands a closer examination. While estimates vary, studies paint a concerning picture, with rates ranging from 15% to 30%, significantly exceeding the national average of 10-15%.
Background:
Postpartum depression is a mood disorder characterized by feelings of sadness, anxiety, and exhaustion experienced by women after childbirth. In South Asia, where cultural norms often prioritize family harmony and the well-being of children, PPD can be particularly challenging due to stigma, lack of awareness, and traditional gender roles.
Factors Influencing PPD in South Asian Women:
Gender Roles: Traditional gender roles in South Asian societies often place significant pressure on women to fulfill domestic responsibilities while neglecting their own mental health needs. The expectation to be the primary caregiver for children exacerbates feelings of stress and inadequacy, contributing to PPD.
Male Child Preference: In cultures where the birth of a male child is highly valued, women who give birth to female infants may experience increased vulnerability to PPD due to societal expectations and pressure from family members.
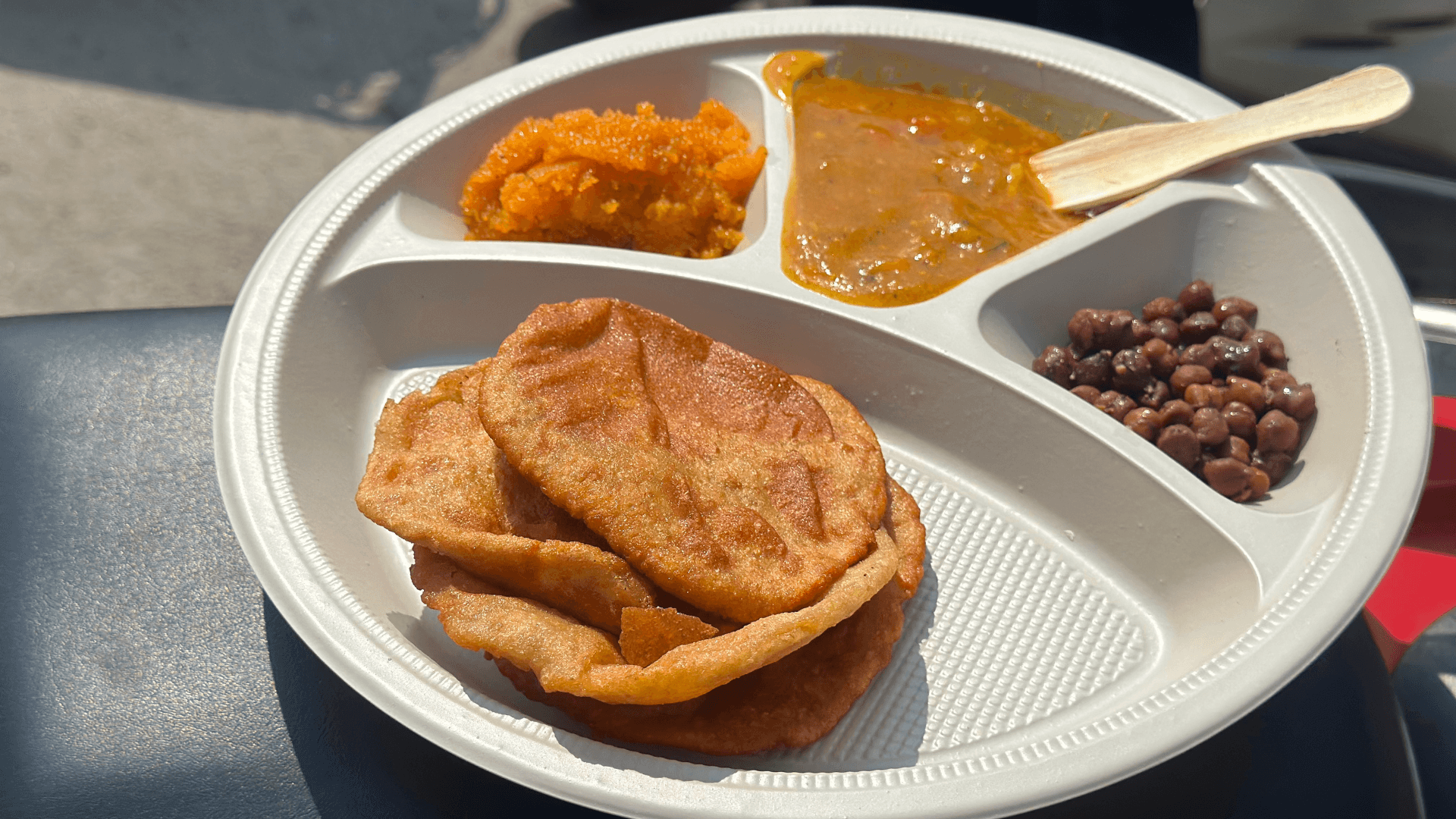
Rituals Regarding Birth: Cultural practices surrounding childbirth, such as postpartum confinement and rituals related to infant care, can impact a woman's mental health. While some rituals may provide social support, others may exacerbate feelings of isolation and anxiety.
Cultural Constraints: Socioeconomic Burdens, Financial stresses, particularly prevalent among immigrant communities, can exacerbate the challenges of motherhood. Limited access to quality healthcare, including mental health services, further complicates timely and effective interventions. Acculturative stress, arising from adapting to new cultural norms or navigating conflicting expectations, creates another layer of strain.
Biological Vulnerability: While biological factors contribute to PPD across populations, it's crucial to acknowledge that specific genetic or hormonal variations might heighten risk within certain groups.
Consequences for Mother and Child:
Untreated PPD can have profound consequences for both mother and child:
Maternal Impact: Emotional unavailability due to PPD can hinder bonding and interaction with the child, potentially impacting their emotional development. Research suggests an increased risk of insecure attachment styles, which can have long-term effects on children's emotional and behavioral well-being. Furthermore, mothers with PPD may struggle with parenting tasks, leading to greater stress and frustration.
Child Development: Studies indicate links between maternal PPD and impaired cognitive development in children, particularly in language and motor skills. Additionally, children of mothers with PPD are more likely to experience behavioral problems like anxiety and aggression.
Shifting the Narrative:
Addressing this issue requires a multifaceted approach:
Transforming Gender Roles: Promoting gender equality, through shared childcare responsibilities and open communication within families, can significantly reduce the burden on mothers.
Culturally Sensitive Support: Developing community-based interventions designed with input from South Asian women and healthcare professionals can ensure culturally relevant and accessible support systems.
Reframing Expectations: Challenging unrealistic societal expectations surrounding motherhood can create a more supportive environment for mothers struggling with PPD.
Targeted Research: Further research is necessary to understand the specific cultural and social factors contributing to PPD in South Asian communities. Investigating the effectiveness of culturally adapted interventions and mental health services tailored to this population is crucial.
Long-Term Impact: Longitudinal studies exploring the long-term impact of PPD on child-mother relationships and child development are needed to inform preventive and intervention strategies.
Treatment Options:
The stigma surrounding mental health within many South Asian communities discourages open discussions, often leading to delayed diagnoses and treatment. The intense pressure to prioritize and sacrifice for childrearing, fueled by strong cultural expectations of motherhood, can leave women feeling overwhelmed and isolated. Additionally, traditional practices may limit social interactions, further restricting access to emotional support networks.
Addressing PPD among South Asian women requires a multifaceted approach that acknowledges cultural nuances and barriers to care. Treatment options may include:
Psychotherapy: Cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT) are effective in treating PPD by addressing negative thought patterns, improving coping skills, and enhancing social support.
Pharmacotherapy: Antidepressant medication may be prescribed in severe cases of PPD, but caution must be exercised due to potential cultural stigma and concerns about breastfeeding.
Support Groups: Peer support networks and community-based interventions tailored to the needs of South Asian women can provide valuable emotional support and validation.
Empowering Change:
By delving into the prevalence, root causes, and consequences of PPD among South Asian women, we can move towards comprehensive solutions. Through collaborative efforts – involving researchers, healthcare professionals, community leaders, and women themselves – we can cultivate a supportive environment that empowers women to seek help, access effective treatment, and nurture healthy relationships with their children. This requires not only addressing individual needs but also tackling broader societal and cultural factors that contribute to the vulnerability of South Asian women in the postpartum period.