Feb 14, 2024
This article discusses weight management for South Asians, focusing on genetic and lifestyle factors increasing their risk of metabolic disorders. It covers genetics, nutrition, psychology, activity, and treatment criteria, emphasizing the need for tailored approaches to improve health outcomes.
South Asians, constituting a significant portion of the global population, face heightened risks of diabetes and heart disease compared to other ethnic groups. Despite similar body mass indexes (BMIs) to Europeans, South Asians exhibit distinct genetic predispositions and lifestyle factors that necessitate tailored approaches to weight management.
Genetics & Health Risks:
Studies reveal higher body fat percentages and increased visceral fat among South Asians compared to Europeans, irrespective of BMI.
South Asians are genetically predisposed to store more visceral fat (the harmful fat around organs) even at lower BMIs. This increases their risk of diabetes, heart disease, and other metabolic issues compared to other populations.
Key genetic risks include higher levels of lipoprotein(a) and larger fat cells, contributing to metabolic syndrome.
Epigenetics & Early Life Influences:
Epigenetic factors, influenced by prenatal environments, contribute to long-term health implications such as central obesity and cardiometabolic diseases among South Asians born with low birth weights.
Low birth weight coupled with rapid childhood weight gain increases susceptibility to metabolic disorders in adulthood.
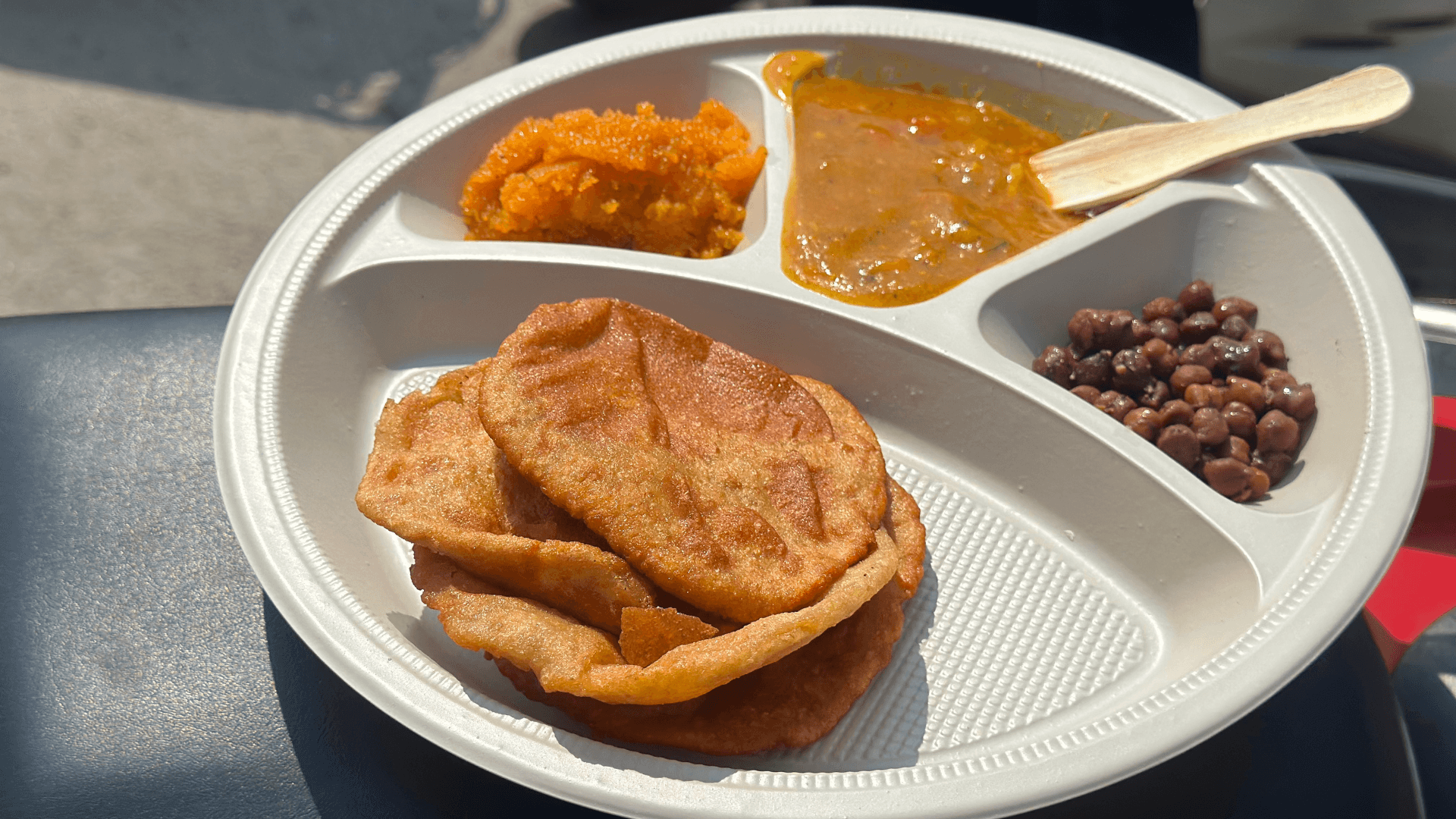
Dietary Challenges:
Traditional South Asian diets often incorporate simple carbohydrates like white rice and flatbreads, fried foods, and may lack protein, leading to metabolic problems.
Dietary patterns characterized by high consumption of simple carbohydrates, fried foods, and sweets contribute to elevated risks of metabolic syndrome and diabetes among South Asians.
Even Canadian-born South Asians can be susceptible, often consuming more processed foods, sugar-laden drinks, and fast food than individuals in their native countries.
Shifts towards processed foods and increased sugar intake further exacerbate metabolic issues in South Asian populations.
Psychological Factors:
Cultural acceptance of overweight individuals differs between genders, potentially leading to higher internalized biases and mental health issues among overweight South Asians.
Stigma towards overweight women can be particularly harsh, leading to self-blame, isolation, and mental health concerns.
Physical Activity & Muscle Composition:
South Asians, on average, engage less in organized sports and vigorous exercise compared to other populations.
Many hold sedentary jobs, and first-generation immigrants facing long working hours and stress are further prone to inactivity.
Notably, research shows Asian Indians with a normal BMI have less muscle mass compared to Europeans with a similar BMI. This highlights the importance of muscle-building exercise for South Asians.
Treatment Considerations:
Due to the higher risks at lower BMIs, South Asians should consider active weight management earlier than other populations.
The "three pillars" of treatment - nutrition, exercise, and psychological support - are crucial.
Medications can be considered at lower BMIs (25+) if metabolic or mechanical conditions (high blood pressure, sleep apnea) are present, or for prevention at higher BMIs (27+).
Bariatric surgery may be considered at a lower BMI (32.5+) compared to other populations, especially with weight-related diseases.
Despite lower "bad" cholesterol, South Asians face a heightened heart disease risk due to their unique lipid profile. This paradox boils down to three key factors:
Undersized defenders: Even at normal levels, their "good" cholesterol (HDL) particles are smaller, offering less protection against harmful cholesterol.
Metabolic fuel: Elevated triglycerides, often linked to metabolic syndrome, act like fuel for heart disease, amplifying the risk.
Genetic time bomb: Higher levels of Lipoprotein(a), a genetic predisposition, independently increase heart disease risk, adding another layer of complexity.
Given the unique genetic, epigenetic, and socio-cultural factors influencing weight management among South Asians, tailored approaches focusing on nutrition, physical activity, and early intervention strategies are imperative to mitigate the heightened risks of metabolic disorders and improve long-term health outcomes.