Jan 23, 2024
This article explores how global health trends and local practices reshape experiences of chronic illness in South Asia. It highlights the rise of medical pluralism, where patients blend traditions with biomedicine, and challenges us to move beyond fixed ideas of "chronic" to embrace the dynamic realities of illness in diverse contexts.
The dynamic and shifting nature of chronicity is brought to the forefront, challenging conventional distinctions between acute and chronic illnesses, especially in the wake of emerging findings on 'long COVID.'
An Reflexive Examination
At the heart of this special issue lies a reflexive examination of the terms 'chronic' and 'chronicity' itself. Scholars question the hegemonic conceptualization of chronicity in public health discourses, cautioning against the potential danger of essentializing patients. The contributions within this issue propose innovative ways of thinking about risk, emphasizing structural factors influencing the chronicity and recursivity of chronic conditions.
Negotiating Lifestyle Disorders
The tendency towards individualization in managing chronic conditions is scrutinized, revealing how responsibilization discourses often prioritize individual choice without considering structural constraints. The papers invite reflection on the constraints and negotiations within which individuals seek to manage their chronic conditions, challenging conventional notions of 'control.'
Unpacking Chronic Tensions in Pakistani Women's Reproductive Health
Ayesha Varley's paper shifts the focus to women's reproductive health in Pakistan, exploring how vaginal discharge, commonly diagnosed as leucorrhea, becomes a symbol of the chronic tensions women face regarding fertility and their overall well-being. Pakistani women navigate between the biomedical diagnosis and a more social understanding of leucorrhea as a manifestation of the "chronic tensions" and inequalities embedded in their daily lives. Varley's work demonstrates how women utilize the term "weeping wombs" as a language of distress and a way to legitimize their need for care, revealing the complex interplay between medical diagnoses and social realities in shaping women's experiences of chronic conditions.
Chronic Lifestyles, Infertility, and the Discourse of 'Chronic Care' in India
Finally, Sharmila Majumdar's research examines the association between infertility and "chronic lifestyles" in middle and upper-middle classes in India. This association, propagated by certain discourses, presents infertility as inevitable and chronic, requiring "chronic care" through assisted reproductive technologies (ARTs). Majumdar exposes the moral judgments embedded in such discourses, where unhealthy lifestyles are blamed for infertility, placing the burden of responsibility on individuals. This highlights the need to critique the power dynamics within medical discourses and consider the social and cultural contexts that shape individual experiences of chronic conditions.
Global Currents and Local Responses to Chronicity
Across these diverse studies, several common threads emerge. Firstly, global discourses on risk and lifestyle related to chronic conditions are demonstrably reshaping local thresholds for what constitutes "illness." Secondly, these global influences are leading to significant changes in local healthcare practices, as communities grapple with adapting to and negotiating with these external forces. Moreover, the continuing relevance of medical pluralism is evident in patients and practitioners creatively amalgamating different medical systems to manage chronic conditions. However, this pluralism is not without its tensions, as debates over evidence, efficacy, cultural identity, and knowledge politics arise within these mixed healthcare landscapes.
Factors Influencing Chronicity:
Socioeconomic disparities: Poverty, lack of access to quality healthcare, and limited education can exacerbate chronic conditions and hinder effective management. Research by Chandrasekhar and Karan (2020) highlights how socioeconomic inequalities in India lead to unequal access to preventive care and chronic disease management, perpetuating chronicity.
Environmental concerns: Pollution, poor sanitation, and climate change contribute to the rise of chronic respiratory illnesses, cardiovascular diseases, and mental health issues. Studies like D'Souza et al. (2017) link air pollution in Delhi to increased asthma prevalence, demonstrating the environmental dimensions of chronicity.
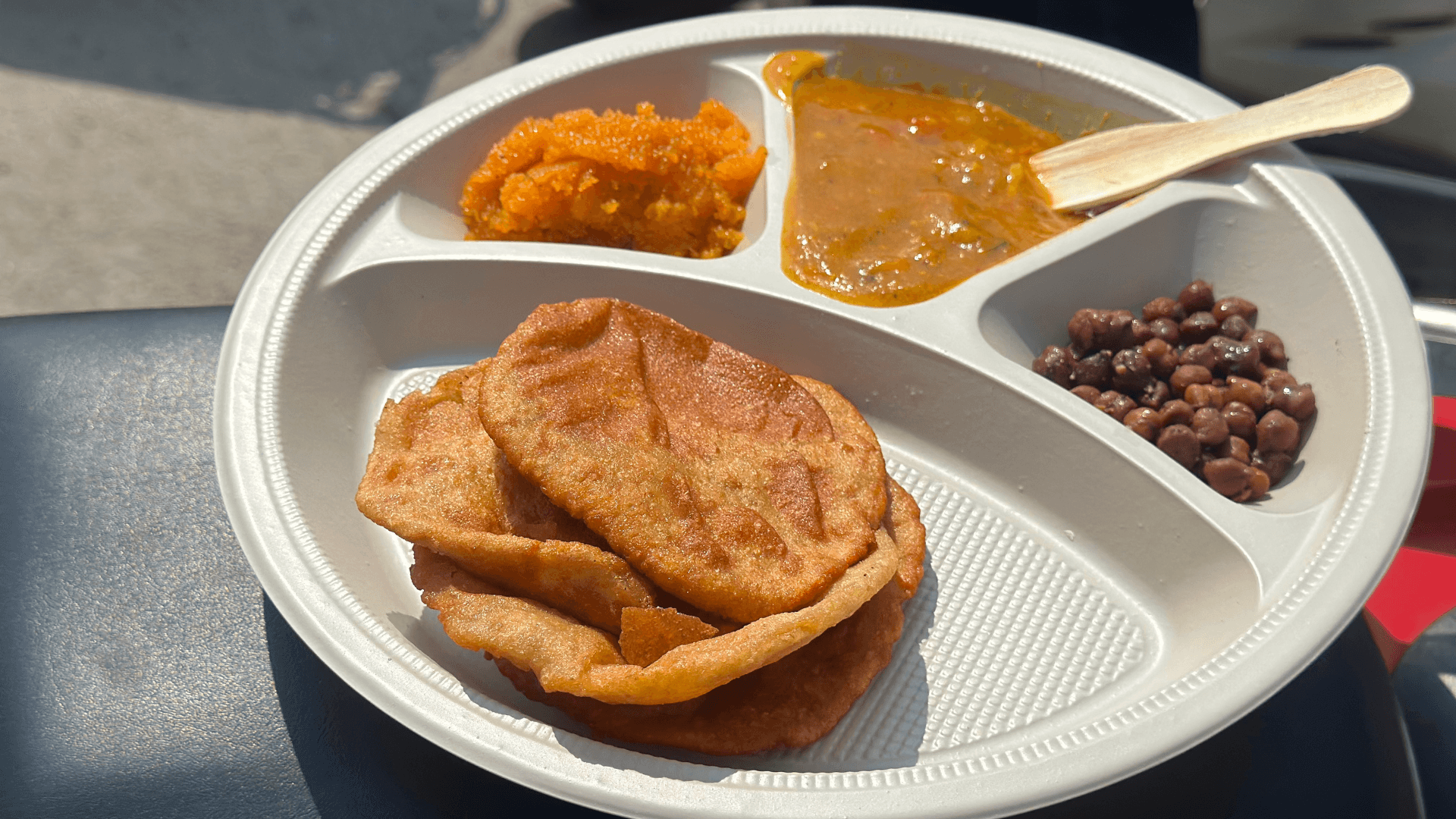
Dietary shifts: Westernized diets high in processed foods, sugar, and unhealthy fats are implicated in rising obesity, diabetes, and cardiovascular diseases. Studies like Popkin et al. (2020) document the rapid dietary transition in South Asia, highlighting the need for public health interventions to promote healthy food choices.
Cultural and religious beliefs: Traditional beliefs and practices can influence perceptions of illness and treatment choices. Research by Kleinman (2011) explores how cultural understandings of illness in South Asia can clash with biomedical approaches, necessitating culturally sensitive healthcare strategies.
Additional Research Insights:
Psychosocial factors: Stress, anxiety, and social isolation can exacerbate chronic conditions. Studies like Patel et al. (2011) emphasize the importance of integrating mental health interventions into chronic disease management programs in India.
Gender dynamics: Women disproportionately face chronic conditions like reproductive health issues and mental health struggles due to gender inequalities and social norms. Research by Jehangir et al. (2018) explores the gendered experiences of chronic illness in South Asia, calling for gender-sensitive healthcare policies.
Role of traditional medicine: Ayurveda, Unani, and other traditional systems offer valuable tools for managing chronic conditions. Research by Sharma et al. (2014) shows the effectiveness of Ayurvedic interventions in managing diabetes, highlighting the potential of integrating traditional medicine into mainstream healthcare.
Patient agency and self-management: Empowering patients through education, self-management skills training, and peer support can improve chronic disease outcomes. Studies like Jayaraman et al. (2015) demonstrate the positive impact of self-management interventions on chronic disease control in India.
Rethinking Illness, Control, and the Power of Pluralism
This special issue compels us to move beyond simplistic notions of chronicity and recognize the dynamic interplay of global and local forces in shaping healthcare experiences in South Asia. It challenges us to consider the agency of patients in navigating complex healthcare landscapes, the evolving role of traditional and alternative healthcare systems
By incorporating these additional factors and research insights, we can create a more comprehensive and nuanced understanding of chronicity in South Asia, paving the way for more effective and equitable healthcare interventions.